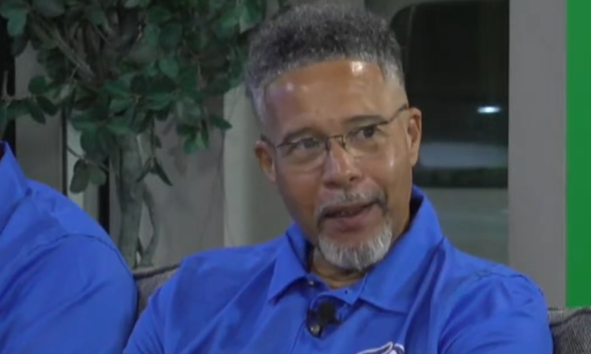
Queen Elizabeth Hospital's New Ophthalmology Department Head, Dr. Trevor Drakes, Addresses Long Waiting Times with Vision for Improved Care
May 31, 2024
New head of ophthalmology at Queen Elizabeth Hospital, Dr Trevor Drakes, aims to reduce long patient appointment and surgery wait times by proposing screening, education for prioritization, and utilizing dormant facilities.
The newly appointed head of the ophthalmology department at the Queen Elizabeth Hospital (QEH), Dr Trevor Drakes, has pledged to address long waiting times for new patient appointments and surgical procedures.
Emphasising the urgent need for change, he outlined his vision in the hospital’s public health talk dubbed Eye in Focus, which he said is to “offer a cure in a timely fashion to the patients because if we’re being honest, that’s not happening at this current moment”.
“There may be long waits for new patient appointments. There are even longer waits for surgical intervention,” he acknowledged.
To reduce delays, the department chief proposed screening new patient referrals and educating healthcare providers on the information required to prioritise cases.
Dr Drakes, a general ophthalmologist, admitted that the wait for cataract surgery is “quite long”, citing the department’s limited capacity as the primary obstacle.
“It’s not because of a lack of expertise but it has to do with the challenges which we face within the QEH. The ophthalmology department still continues to share a single operating theatre where the surgeons are unable to work more than every other week,” he said, suggesting that having another theatre could “easily double” output.
He said he hopes to utilise the long-term dormant third floor of the hospital’s Lion’s Eye Care Centre built more than 30 years ago, which he said “has remained dormant for the last 10 years”.
With an estimated 100 patients visiting the eye clinic daily, Dr Drakes stressed the importance of improving appointment scheduling to manage the high volume efficiently.
“We’ve tried in the past to stagger appointments. It did not work because the patients still continue based on tradition to come at 8.30 am and at 1 pm so we abandoned that,” he said. However, he added: “It’s going to require some education on the part of the QEH and educating patients as to how to keep their appointments.”
To implement his plan, Dr Drakes conceded more staff are needed. “Currently there are four doctors who are actively managing the clinic. That means each clinic session can probably see about 48 patients. There is no eye clinic that has had 48 patients for a very long time. The numbers are double that. So, we definitely need to increase our staff so that we can actually offer more timely care.”
Acknowledging efforts to ensure a functional healthcare system while indicating room for improvement, Dr Drakes concluded: “Timely maintenance programmes, staggered appointments [and] more surgical operating time, and I think we could actually go a long way towards making the public that we serve a lot happier.”


